Oxygen therapy can be lifesaving but nurses must know how it works, when to use it, and how to correctly assess and evaluate a patient’s treatment.
Knowing when to start patients on oxygen therapy can save lives, but ongoing assessment and evaluation must be carried out to ensure the treatment is safe and effective Oxygen is required by all tissues to support cell metabolism; in acute illness, low tissue oxygenation (hypoxia) can occur due to a failure in any of the systems that deliver and circulate oxygen. Hypoxia is an indication to start oxygen therapy; this can be a life-saving intervention, but given without appropriate assessment and ongoing evaluation, it can also be detrimental to patients’ health.
OXYGEN TREATMENT
When used as a medical treatment, oxygen is regarded as a drug and must be prescribed. In 2008, the British Thoracic Society produced guidelines for its use with acutely unwell adult patients (O’Driscoll et al, 2008). This was endorsed by 21 professional groups across a wide range of professions and specialties.
The guidelines recommend:
- Administering oxygen to treat hypoxemia (low blood oxygen levels);
- Prescribing a target oxygen saturation range to guide therapeutic treatment.
Oxygen does not treat breathlessness in the absence of hypoxemia
In an emergency situation, immediate assessment of airway patency, breathing and circulation is essential, and in critical illness such as peri-arrest, high-concentration oxygen should be commenced via reservoir mask at 10-15L/min if the patient is hypoxic, with continuous monitoring of pulse oximetry and prescription of an appropriate target range once the patient’s condition is stabilized.
The target saturation range is prescribed according to the patient’s condition. For most patients, a target of 94-98% is appropriate. For those at risk of carbon dioxide retention (hypercapnia), a target of 88-92% ensures safe levels of oxygenation and minimizes risk of respiratory acidosis.
Those at risk include patients with:
- Chronic obstructive pulmonary disease (emphysema);
- Neuromuscular and chest wall disorders;
- Cystic fibrosis;
- Morbid obesity.
Pulse oximetry must be available in all settings where emergency oxygen is used. It is essential to:
- Record inspired oxygen (FiO2), delivery device and oxygen saturations;
- Monitor and document the effect of any changes to administered oxygen therapy.

DELIVERY DEVICE
Oxygen is delivered via variable-performance or fixed-performance devices.
Variable-performance devices
The amount of oxygen delivered by variable-performance devices (also known as uncontrolled oxygen systems) is dependent on the:
- Oxygen flow rate;
- Patient’s inspiratory volumes;
- Respiratory rate;
- Proportion of room air added during breathing.
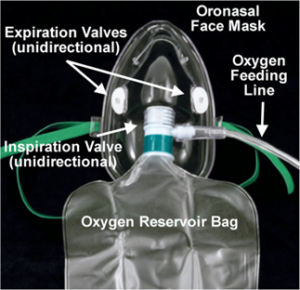
Reservoir mask (non-rebreathing mask)
Oxygen at 10-15L/min via a reservoir mask delivers oxygen at concentrations of 60-85% and is recommended for short-term use in patients who are critically ill.
The reservoir bag must be filled with oxygen before use and the mask positioned to ensure a close fit on the patient’s face. A one-way valve prevents exhaled air entering the bag.
Oxygen via a reservoir mask cannot be humidified, and patients will be more comfortable if they can be maintained within target range on a humidified system once they are more stable.

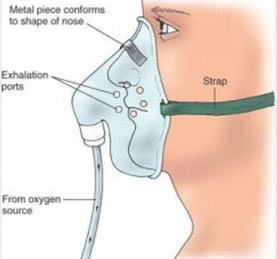
Simple face mask
The simple, or “low flow”, face mask is intended for short-term use, such as post-operative recovery. Oxygen is delivered at 2-10L/min and supplemented with air drawn into the mask during breathing.
The FiO2 achieved cannot be predicted as it depends on the rate and depth of the patient’s breathing. Oxygen flow rates of <5L/min may result in the patient rebreathing exhaled carbon dioxide, which may build up in the mask. Simple face masks should not be used for patients at risk of type 2 respiratory failure.

Nasal cannula
Nasal cannula are comfortable and well tolerated by most patients. They do not need to be removed when the patient is talking or eating. Oxygen is inhaled even when breathing through the mouth. Nasal cannula are useful:
- For patients who are stable;
- To provide supplemental oxygen therapy during meals;
- To provide air-driven nebulized therapy for those requiring controlled oxygen therapy.
- They are commonly used to deliver oxygen in the home setting.
Flow rates above 4L/min can cause considerable drying of nasal mucosa and are more difficult to tolerate. The FiO2 achieved varies with the rate and depth of breathing and, therefore, nasal cannula should not be used in patients with unstable type 2 respiratory failure.


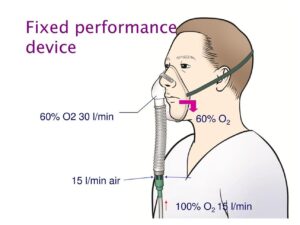
Fixed-performance devices
Fixed-performance devices (also known as controlled oxygen delivery systems) deliver a fixed proportion of air and oxygen via a Venturi valve, ensuring an accurate concentration of oxygen is delivered, regardless of inspiratory volumes and respiratory rate. Fixed-performance devices should be used in acute illness in patients who are at risk of carbon dioxide retention.
The minimum flow rate varies between oxygen-mask manufacturers, so it is important to check the minimum rate that is recommended on the device in use.
If patients are extremely breathless but achieving adequate oxygen saturation rates, increasing the oxygen flow rate by 50% (for example, increasing from 2L/min to 3L/min) will increase the gas flow into the mask without increasing the percentage of oxygen delivered, and may be more comfortable for them.
Starting oxygen therapy
The following procedure should be followed when starting oxygen therapy in patients who are acutely ill:
- Ensure pulse oximetry is available to monitor response to oxygen therapy
- Document baseline observations including saturations, respiratory rate, blood pressure and pulse
- Note respiratory effort, colour, level of consciousness
- Check that there is a prescription for oxygen with a stated target saturation range (except in peri-arrest situation)
- Where there is no known risk of carbon dioxide retention (target 94-98%), start oxygen therapy using a reservoir mask at 10-15L/min. Where there is a risk of carbon dioxide retention (target 88-92%), start oxygen therapy using a 28% Venturi device and mask
- Ensure delivery device is connected via tubing to oxygen supply and turned on to the appropriate flow rate (if cylinder, check fill level of cylinder and be aware of duration time)
- Explain procedure to the patient and gain consent where possible. In patients who are acutely sick, this may not be possible and clinicians should act in the patient’s best interests
- Place the oxygen mask on the patient’s face, adjusting the nose clip and elastic straps to ensure a close fit
- Reassure the patient – if the patient is very breathless, oxygen masks can feel very claustrophobic
- Monitor response to oxygen therapy – recheck oxygen saturations, vital signs, colour and level of consciousness
- Titrate oxygen according to oxygen saturations (Fig 4) to maintain saturations within prescribed target range. Allow five minutes at each dose before further adjustment. Sudden withdrawal of oxygen in a patient with hypercapnia leads to rebound hypoxaemia
- Document all adjustments to inspired oxygen (FiO2), with saturations recorded.
Ongoing care of patients requiring oxygen therapy in the acute setting(Home)
- Continue to monitor oxygen saturations at least four times a day. Always record saturations at rest and document FiO2 in situ at the time
- Patients requiring >28% oxygen for more than 24 hours can have oxygen delivered via a humidification system for comfort and to avoid the drying of secretions
- Stable patients may be more comfortable with nasal cannulae but care must be taken to ensure saturations remain in the target range
- Patients requiring increasing doses of oxygen to maintain saturations within range, or with signs of respiratory deterioration (increasing respiratory rate, drowsiness, headache, tremor, increasing early warning score) require prompt medical review and further assessment including monitoring of arterial blood gas
- Help the patient to stay in an upright position to maximise ventilation unless contraindicated by underlying clinical problems, for example, spinal or skeletal trauma
- Give other prescribed therapies, such as nebulised bronchodilation, diuretics, ventilatory support
- Refer for respiratory physiotherapy if patients have difficulty clearing thick secretions
- Observe potential pressure areas, particularly behind the ears, from nasal cannula tubing or mask elastic and ensure skin is protected and pressure is relieved by altering the position of the tubing or using padding
- Be aware of the drying effect of oxygen on oral and nasal mucosa; encourage patients to maintain adequate oral fluid intake where appropriate, and provide water-based lubricant gel to relieve nasal drying. Do not use oil-based preparations such as Vaseline or petroleum jelly
- Consider discontinuing oxygen therapy once the patient has stable saturations (at least two consecutive recordings) within their target range on low-dose oxygen (for example, 1-2L/min via nasal cannula). Monitor saturations for five minutes after stopping oxygen and recheck after one hour
Key points
- Hypoxia is an indication that oxygen therapy should be started
- If blood oxygen levels are not low, oxygen will not treat breathlessness
- A target oxygen saturation range should be prescribed to guide therapy
- A lower target saturation range should be prescribed for patients at risk of hypercapnia
- The amount of oxygen received by the patient is dependent on the delivery device used; ensure appropriate device is selected


